Infant jaundice is a common condition. Specially this may occur in babies born before 38 weeks gestation and some breastfed babies.
What is new born jaundice?
Yellow discoloration of a newborn baby’s skin and eyes. It is usually occurring because a baby’s liver is not fully developed. So, it is less effective at removing bilirubin from the blood stream. Sometimes this may occur due to an underlying disease. There are three types of jaundice.
- Physiological Jaundice
This type of jaundice is very common in new born babies and goes away its own after 2-3 days when the baby’s liver matures enough to get rid of excess bilirubin from the blood.
- Breastfeeding Jaundice
This is also a common condition in breastfed babies in the baby’s first week after born. The reasons are sucking difficulties of babies, not enough breast milk producing by mom or mistakes of nursing techniques. This may take some times to recover but goes away after breastfeeding established.
- Breast Milk Jaundice
Composition of your breast milk can determine how your baby’s liver breaks down the bilirubin. This type of jaundice has been known to run in families. This is most often occurring in the second or later weeks of life and can continue for several weeks. Usually, breast milk jaundice spontaneously resolves even without discontinuation of breastfeeding.
Causes of Jaundice in Newborn
As mentioned above, most common cause for the jaundice is excess bilirubin in infant blood. There are some other causes or diseases that can cause in babies. Those are,
- Internal bleeding
- An infection in blood (Sepsis)
- Other viral or bacterial infections
- An incompatibility between your blood and the baby’s blood
- A liver malfunctions
- A liver condition such as Biliary atresia
- An enzyme deficiency
- A low oxygen level Chypoxia
- An abnormality of your baby’s red blood cells that causes them to break down rapidly
Risk Categories
- Most commonly 80% of premature babies gets infant jaundice due to difficulties of breakdown bilirubin or less bilirubin eliminated through stool as they have fewer bowl moments.
- When the baby’s blood type is different from the mother’s blood type baby will get antibodies through placenta causing rapid break down of red blood cells.
- If the baby gets bruising during the delivery, they may get jaundice due to breakdown of more red blood cells.
- Difficulties of breastfeeding will lead to lack of nutrition. So, dehydration or a low caloric intake may contribute to infant jaundice.
- According to study done on 2002, neonatal jaundice occurred more often among East Asian and mixed Asian/white infants than among white infants.
Symptoms of Jaundice
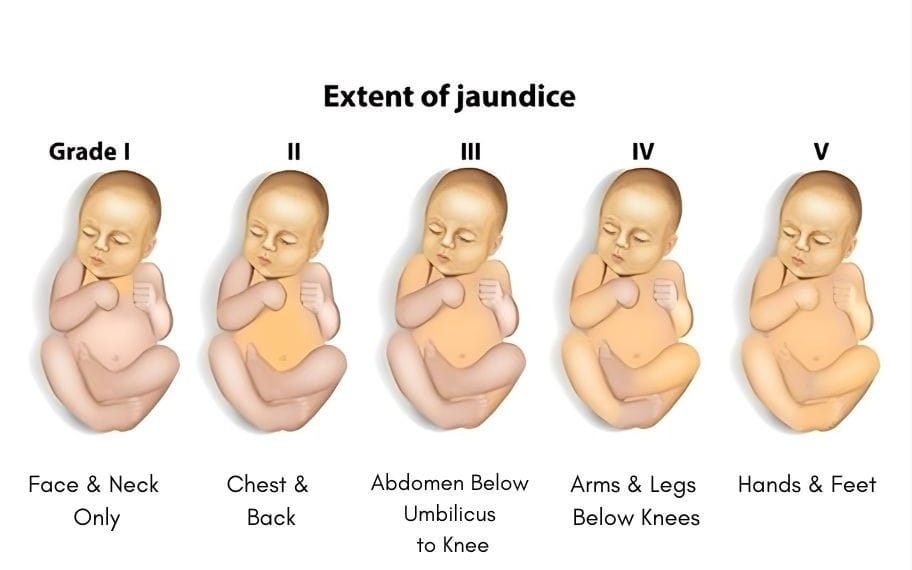
Most common symptom is yellowing of a baby’s skin and white of eyes. This may appear within 2 to 4 days after birth. Yellow color usually appearing first on the face and scalp then to the white parts of the eyes (sclera) and spreading to the skin of the body (in moderate jaundice). Finally, palms of the hands and soles of the feet turning yellow (in severe jaundice).
Other symptoms are;
- Baby is listless or sick and difficult to awaken
- Baby makes high-pitched cries
- Baby isn't gaining weight or is feeding poorly
- In some cases, light-colored stool and dark urine
How to Diagnose the Jaundice?
You can check for infant jaundice in good lightning conditions by pressing gently on your baby’s skin. If the skin turns simply lighter color than its normal color for a moment you baby does not have jaundice. If the skin turns yellow, it is likely a sign of jaundice.
This clinically diagnose by
- Complete Blood Count (CBC)
- Blood type
- Rh factor incompatibility
- Coombs test: This test checks your blood for antibodies that attack red blood cells
Prevention
The best way to prevent infant jaundice is adequate feeding. Breast fed infants should have 8 to 12 times feeding per day. Formula fed babies usually should have 1 to 2 ounces (30 to 60ml) of formula every 2-3 hours for the first week. This ensures that your baby is not dehydrated and helps bilirubin pass through their body more quickly.
When to See a Doctor?
Most of the time jaundice is harmless and goes away its own. But sometimes severe jaundice can increase the risk of bilirubin passing in to the brain which can cause permanent brain damage. Visit your doctor if;
- Your baby’s skin become more yellow
- The whites of your baby’s eyes look yellow
- Baby develops a fever over 100 0F (38 0C)
- Baby feeds poorly, appears listless or lethargic and makes high-pitched cries
- Isn’t gaining weight
Treatments
- Phototherapy
During phototherapy expose your baby's skin to as much light as possible. Your baby will be placed under a light with their eyes covered. You can feed your baby and change their nappy while the phototherapy stops for 30 minutes. If your baby's jaundice does not improve, intensified phototherapy may be offered. In here the amount of light will increased using another source of light, such as a light blanket, at the same time. This treatment cannot be stopped for breaks during intensified phototherapy, so you will not be able to breastfeed or hold your baby. But you can give your baby expressed milk.
During phototherapy, you baby's temperature will be measured in time to time, to make sure they're not getting too hot, and they'll be checked for any signs of dehydration. Phototherapy will be stopped when the bilirubin levels fall to a normal level.
An Exchange Transfusion
Rarely, a baby may need an exchange transfusion of blood as severe jaundice doesn't respond to other treatments. This involves withdrawing small amounts of blood through a thin plastic tube placed in blood vessels in their umbilical cord, arms or legs and replacing it with donor blood, diluting the bilirubin and maternal antibodies. Your baby's blood will be tested within 2 hours of treatment to check if it's been successful. If it is not successful, the procedure may need to be repeated.